Anaemia in pregnancy
Anemia in pregnancy
Anemia in pregnancy is defined as a hemoglobin concentration of less than 110 g/L (less than 11 g/dL) in venous blood.
It affects more than 56 million women globally, two-thirds of them being from Asia. Although more prevalent in less-resourced countries, women from developed countries are also affected. Women from both rural and urban areas are vulnerable.
The global prevalence of anemia in pregnancy is estimated to be approximately 41.8%, varying from a low of 5.7% in the USA to a high of 75% in The Gambia.
A large number of women from less-resourced countries embark upon pregnancy with frank iron deficiency anemia and/or depleted iron stores. Anemia is the major contributory or sole cause in 20–40% of maternal deaths.
Effects of anemia on mother
Women with mild or moderate anemia often tend to be asymptomatic and anemia is detected on screening alone. As anemia advances, the symptoms of fatigue, irritability, generalized weakness, shortness of breath, frequent sore throats, headache (frontal), brittle nails, pica (unusual craving), decreased appetite and dysphagia (owing to postcricoid oesophageal web) may occur. Clinical signs of anemia include pallor, blue sclera, pale conjunctiva, skin and nail changes, leg edema, gum and tongue changes (glossitis and stomatitis), tachycardia and functional heart murmur .
Effects of anemia in pregnancy
Anemia increases perinatal risks for mothers and neonates; and increases overall infant mortality. The odds for fetal growth restriction and low birth weight are tripled. The odds for preterm delivery are more than doubled. Even a moderate hemorrhage in an anemic pregnant woman can be fatal.
Effects of anemia on fetus and neonate
A basic principle of fetal/neonatal iron biology is that iron is prioritized to red blood cells at the expense of other tissues, including brain. When iron supply does not meet iron demand, the fetal brain may be at risk even if the infant is not anemic. Although dietary deficiency may be contributory, the etiology of the vast majority of cases of iron deficiency anemia in infancy and childhood is maternal iron deficiency anemia in pregnancy. Anemia adversely affects cognitive performance, behavior and physical growth of infants, preschool and school-aged children. Anemia depresses the immune status and increases the morbidity from infections in all age groups. It adversely impacts the use of energy sources by muscles and thus the physical capacity and work performance of adolescents and adults.
Diagnosis of anemia in pregnancy
This may be suggested by
The symptoms and clinical signs.
A hemoglobin (Hb) 11 g/dL or hematocrit of <33% can be considered for diagnosis of anemia in pregnancy.
Iron deficiency anemia is characterized by low mean corpuscular volume (MCV), low mean corpuscular hemoglobin concentration (MCHC) and low ferritin levels. Peripheral smear shows hypochromic microcytic red cells. Severe anemia in pregnancy (Hb <7 g/dL) requires urgent medical treatment and Hb <4 g/dL is an emergency carrying a risk of congestive cardiac failure, sepsis and death.
Causes of anemia in pregnancy
Physiological adaptation in pregnancy leads to physiological anemia of pregnancy. This is because the plasma volume expansion is greater than red blood cell (RBC) mass increase which causes hemodilution.
Normal pregnancy increases iron requirement by 2–3 fold and folate requirement by 10–20 fold. Major causes of anemia are:
Nutritional – iron, folate and vitamin B12 deficiencies Acute or chronic blood loss (gastrointestinal bleeding/heavy periods)Infections – malaria, HIVChronic diseases – renal, neoplasia Parasites Hemolytic anemias – drugs, congenitalHemoglobinopathies – sickle cell, thalassemia
Nutritional iron deficiency anemia (IDA) is the commonest (90%) cause of anemia in pregnancy. IDA is associated with increased maternal and perinatal morbidity and mortality, and long-term adverse effects in the newborn. A 55-kg pregnant woman is estimated to need approximately an additional 1000 mg of iron over the whole pregnancy. It has been estimated that the daily iron requirements of a 55-kg pregnant woman increases from approximately 0.8 mg in the first trimester to 4–5 mg during the second trimester and >6 mg in the third trimester.
Pregnant women need iron to cover their basic losses, increased RBC mass and demand from fetoplacental unit. This requirement is not met by food alone in developing countries and oral iron supplementation is justified.
Prevention of anemia in pregnancy
Pre-pregnancy counseling, dietary advice and therapy is very important for ensuring best pregnancy outcomes.
It is recommended that full blood count should be checked at the booking visit in pregnancy and repeated at 28 weeks to screen for anemia.
In high risk mothers and multiple pregnancies, an additional hemoglobin check should be performed near term. Dietary advice should be given to all mothers to improve intake and absorption of iron from food.
Rich sources of iron include heme iron (in meat, poultry, fish and egg yolk), dry fruits, dark green leafy vegetables (spinach, beans, legumes, lentils) and iron fortified cereals.
Using cast iron utensils for cooking and taking iron with vitamin C (orange juice) can improve its intake and absorption. Certain foods which may inhibit iron absorption should not be taken with iron rich foods. These include polyphenols (in certain vegetables, coffee), tannins (in tea), phytates (in bran) and calcium (in dairy products). Weekly iron (60 mg) and folic acid (2.8 mg) should be given to all menstruating women including adolescents, periodically, in communities where IDA is considered a problem.
Increased intake of iron, treatment of underlying conditions like deworming (anti-helminthic therapy) are important preventive measures. Pregnant women need iron to cover their basic losses, increased RBC mass and demand from fetoplacental unit.
Vitamin B12 and folate deficiencies in pregnancy are rare and may be a result of inadequate dietary intake with the latter being more common.
These vitamins play an important role in embryogenesis and hence any relative deficiencies may result in congenital abnormalities. Finding the underlying cause is crucial to the management of these deficiencies. From a neonatal perspective, delayed clamping of the umbilical cord at delivery (by 1–2 min) is important step in prevention of neonatal anemia.
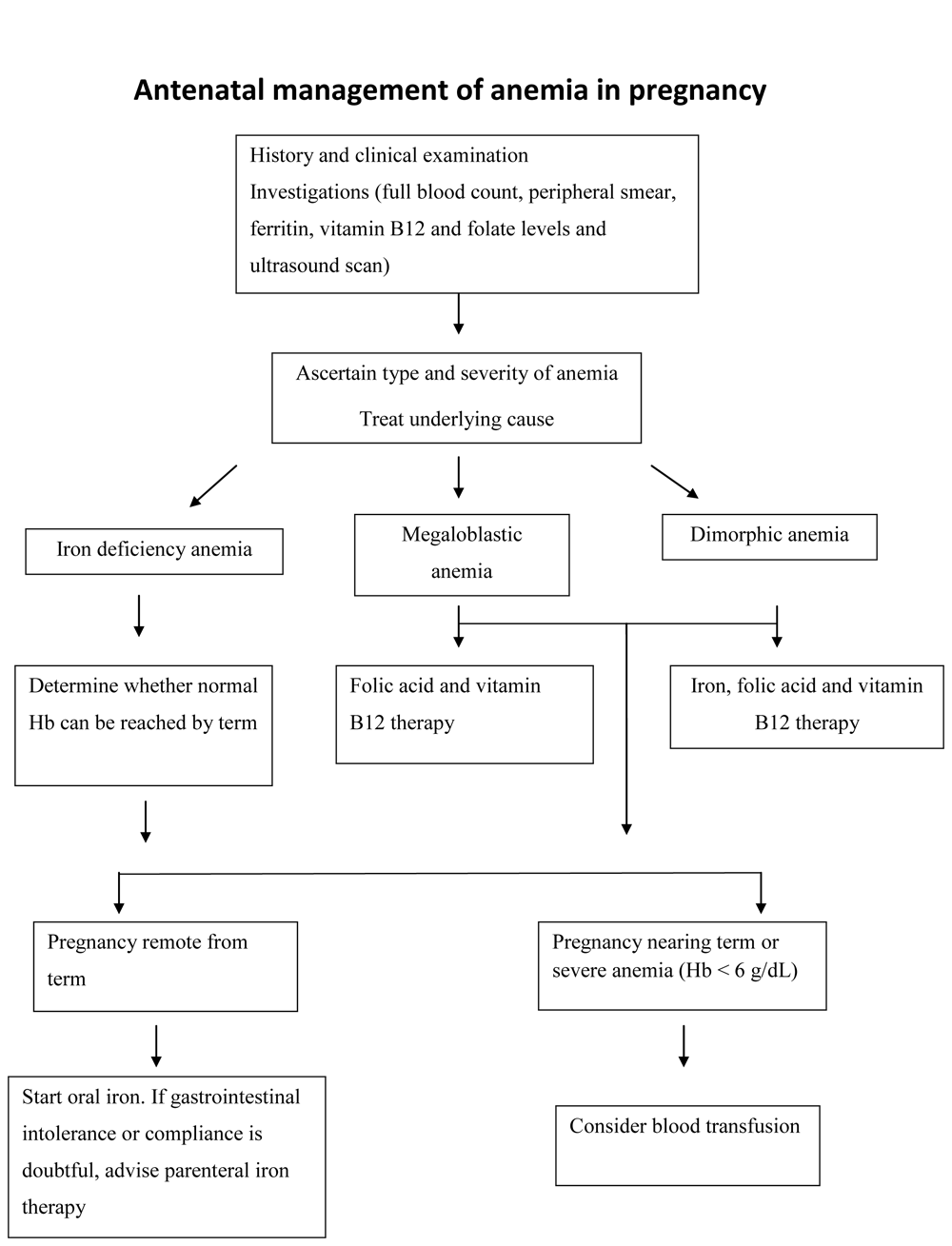
Treatment of anemia
Correction of iron deficiency in pregnancy involves appropriate diet and oral iron supplementation. Daily oral iron (60 mg) and folic acid (4 mg) should be commenced as soon as possible together with behavior changing communications when a woman becomes pregnant, and continued up to 6 months' postpartum.
The dose of iron could be reduced to 30 mg in women who have no IDA. The aim is to achieve a hemoglobin of at least 10 g/dL at term.
The choice of iron preparation is based on patient tolerance to a large extent. It is recommended to take iron with orange juice to enhance its absorption. Oral ferrous salts are the treatment of choice (ferric salts are less well absorbed).
Ferrous sulphate 200 mg 2–3 times daily (each tablet provides 60 mg elemental iron) is the most common preparation used.
Alternative preparations include ferrous gluconate and ferrous fumarate. In the first week following initiation of iron therapy, there is often no rise in hemoglobin level but reticulocytosis is observed. Hemoglobin level usually starts rising in the second week and the expected improvement in hemoglobin is approximately 1 g/dL per week. Common adverse effects of iron therapy include nausea, constipation and occasionally diarrhea (reduced by taking tablets after meals).
Parenteral iron is required for those not tolerating oral iron or who need rapid correction of anemia (severe anemia in last month of pregnancy) and where oral therapy has failed. Parenteral iron can be administered intramuscular (IM) or intravenous (IV). The main drawbacks of IM route are pain, staining of skin, myalgia, arthralgia and injection abscess. Intravenous iron can be administered as total dose infusion; however, utmost caution is needed as anaphylaxis can occur. Iron dextran and iron polymaltose preparations can be used by both IM and IV routes. Two newer IV preparations – iron sucrose and ferric gluconate are associated with reduced side-effects. Each iron sucrose ampoule contains iron sucrose equivalent to 50 mg elemental iron. Iron sucrose may be administered undiluted by slow intravenous injection at a rate of 1 mL (20 mg iron) solution per minute not exceeding 100 mg iron per injection. It may also be administered by IV infusion. Infusion must be administered as every 2.5 mL iron sucrose diluted exclusively in a maximum of 100 mL of 0.9% NaCl (saline), immediately prior to infusion. The solution must be infused at a rate of 100 mg/15 minutes. Unused diluted solution must be discarded.
Blood transfusion should be considered when a patient has decompensated owing to a drop in hemoglobin concentration and needs a more rapid rise in hemoglobin. Packed red cell transfusion may be indicated for pregnant women with severe anemia (Hb of 6 g/dL or less) close to due date or less than 8 g/dL if they have increased risk of blood loss at delivery.
Folate deficiency is seen in 5% cases of anemia in pregnancy. It is associated with hemolytic anemias, hemoglobinopathies, antiepileptics and poor nutrition. A dose of 5 mg oral folic acid daily is recommended for correction of anemia. In cases of vitamin B12 deficiency, 250 µg cynacobalamin administered parenterally every week is recommended for anemia treatment. In cases of severe anemia near term – daily vitamin B12 in a dose of 100 µg should be administered for a week.
Management during labor
Cross-matched blood should be available if needed in case of significant hemorrhage at the time of delivery. Strict asepsis is very important. In case of severe anemia with congestive cardiac failure, active management of third stage (with methyl ergometrine) is contraindicated.
Postpartum management
Close monitoring should be performed for signs of decompensation, infection or thrombosis. Appropriate thromboprophylaxis and contraceptive advice should be provided and hematinic supplementation should continue.
Recent advances in treatment of anemia
Erythropoetin is the new agent used in treatment of anemia in following situations:
Erythropoietin deficient anemiaSevere or progressing iron-deficiency anemiaJehovah’s Witnesses or other refusal of blood transfusionPlacenta previa (or placenta accreta)Preoperative and postoperative patientsAutologous blood donationHemoglobinopathies.
Erythropoietin is gaining popularity as a therapeutic option during pregnancy and the postpartum period. Further research is needed to establish a standard dosage and dosing interval.
Posted by
Welfare Jambo







Post a Comment